The SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus, which hit China with the disease now named COVID-19 in December 2019 and has since spread to over 70 countries, has caused over 90,000 cases, and 3,117 fatalities, with 95% or more of both being in China.
COVID-19 is being studied intensively, on an unprecedented scale. There have been over 400 published articles, and the viral genome sequence was mapped. The viral characteristics, epidemiological characteristics, and the sickness itself have all been described in detail. The sequencing success allowed the development of diagnostic tests and the initiation of vaccine and therapeutic drug development. The guidelines for clinical and laboratory diagnosis and containment are now updated regularly, while treatment regimens have reached the stage of clinical trials.
The virus
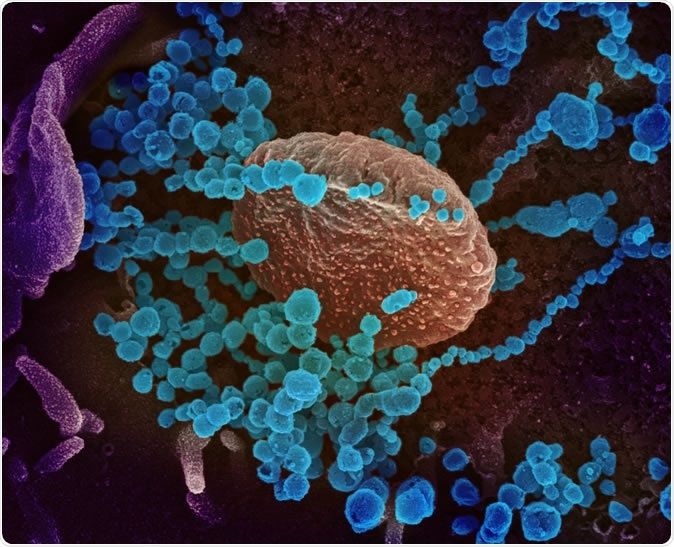
SARS-CoV-2, called 2019-nCoV by the World Health Organization (WHO), is a novel member of the beta coronavirus family that infects humans. It is thought to have come from a bat species called chrysanthemum bats. Its spike (S) receptor enters the host cells to bind to the angiotensin-convertingenzyme2 (receptor in humans. However, specific antibodies that target the receptor-binding domain of the older SARS-CoV do not bind to the new one, showing its novel characteristics.
The ACE2 cells are the receptors found in type II alveolar cells, and perhaps even more commonly and abundantly in Asian males. Smoking could be an even more important determinant in the difference in distribution between men and women.
An intermediate host is likely, possibly the pangolin, within which the bat and pangolin coronaviruses are thought to have recombined to create the novel virus. However, more questions remain unanswered, such as the reason for its sudden emergence, the reasons for its rapid contagion compared to SARS-CoV and MERS-CoV, and the viral components capable of presenting the most significant therapeutic and vaccine targets.
Currently, the incubation period is thought to range from 1-14 days, with the most common period being 5-6 days. It may be as long as 27 days, according to a few researchers, in which case the 14-day quarantine being enforced at present is inadequate. Spread from asymptomatic patients is a possibility, and a single case can produce 2 or 3 secondary cases, which means a reproductive number R0 than for the other SARS virus.
The virus spreads via large droplets but is present in blood and in stools, which may mean that more stringent protection is required to prevent spread, primarily via health care systems, which are a significant player in the chain of transmission – up to 41% according to one study.
Furthermore, finally, scientists estimate that about 2 of every 3 cases of infection that have been carried out of mainland China have escaped detection at present, based on air travel statistics.
The patient
Most patients seem to be in their 50s, and about a quarter have a severe illness justifying intensive medical care. About 1 in 10 will need to be placed on a mechanical ventilator. This picture is based on Wuhan reports, and outside this city, the illness seems milder, especially if the patients are younger.
Over 80% of patients present with fever and dry cough and many have muscle pain and/or tiredness. Many also report headaches, sore throat, abdominal pain, and diarrhea.
The laboratory tests show a deficiency of lymphocytes in 70% of patients, with increased prothrombin time and a high LDH level. Chest CT scans show typical ground-glass opacities, and chest radiographs display patchy infiltrates in both lungs. The scanty autopsy data available indicates hyaline membrane formation, with mononuclear cells infiltrating the lung tissue. The spectrum of the disease remains to be defined more thoroughly, from the most severe to the asymptomatic case.
Case fatality rate is also variable, from 8% to 15% in older patients within Hubei province, and those with other illnesses who went on to show signs of severe lung disease but appears to be within the range of 1% to 2% outside this area. The actual figures will depend on whether mild cases are being detected accurately.
Screening and testing
All people who have traveled to China or had close contact with an individual suspected or known to have COVID-19 within the last 14 days must be screened, according to both WHO and Centers for Disease Control and Prevention (CDC). However, this is likely to be broadened since cases are surging in other countries as well, including Japan, Italy, and South Korea, and some cases have no history of such contact.
Test kits have not measured up to standard in many cases, creating a bottleneck in diagnosis. Despite CDC’s release of data on primers, probes, and test protocols, only a few public health laboratories can carry out the testing, and only about 500 tests have taken place so far in the US, indicating the need for strengthening the testing facilities.
At present, the CDC recommends the use of a nasopharyngeal swab and preferably a sputum sample from the lower respiratory tract, though serum may also be used. The procedures used are reverse-transcriptase polymerase chain reaction (RT-PCR), and often a complete blood count and other routine microbiological parameters including screening for other viruses are also ordered.
Management
COVID-19 patients are treated like other pneumonia patients, mainly with supportive care. Trials of the prodrug remdesivir, which is a synthetic nucleoside analog that inhibits the replication of viral RNA and thus contains the infection, are ongoing. Another drug combination is the lopinavir/ritonavir protocol, which was useful in animals with MERS-CoV, but evidence of human efficacy is still awaited. Another experimental drug being used in China is favilavir, also used for influenza. About 100 trials are being conducted currently to test the efficacy of new as well as repurposed drugs in this epidemic.
Vaccines are still in the pipeline, over 11 of them, and one phase I trial will start in March 2020. Personal protective equipment, the use of universal, comprehensive protection in health care facilities, including airborne protection by an N95 respiratory-face shield/goggles combination or an electrical respirator that delivers pure air. Again, these are not available in required numbers everywhere, and mild or asymptomatic cases escape the net of detection. Improperly executed quarantines are counterproductive, as seen in that imposed on crew and passengers of the ship the Diamond Princess, which resulted in over 700 infections.
The pressing needs of the current epidemic include an effective and rapid diagnostic test, effective therapies, and a safe, potent vaccine.
Story Source:
News Medical. Note: Content may be edited for style and length.